Pain Reprocessing Therapy (PRT): A Comprehensive Overview
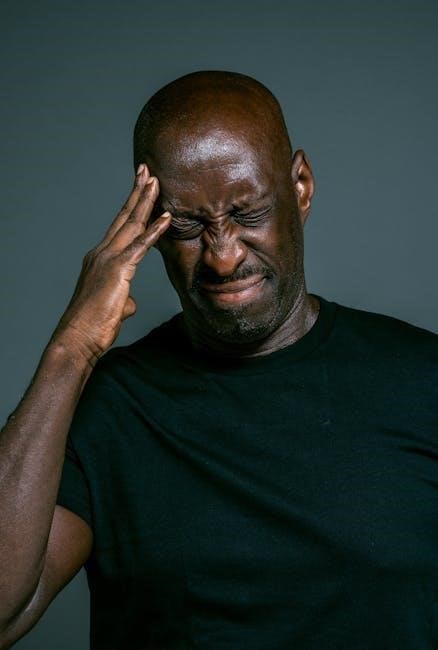
Pain Reprocessing Therapy (PRT) emerges as a promising psychotherapeutic approach, specifically designed to disrupt the detrimental fear-expectation-pain cycle, offering lasting relief.
Recent trials demonstrate remarkable success, with up to two-thirds of patients achieving pain elimination or near-elimination through this innovative treatment modality.
PRT focuses on retraining the brain, accurately identifying bodily sensations, and fostering a less threatening perception of pain signals, ultimately promoting recovery.
What is Pain Reprocessing Therapy?
Pain Reprocessing Therapy (PRT) is an evidence-based therapeutic system utilizing psychological techniques to fundamentally retrain the brain, effectively breaking the cycle of chronic pain. Unlike traditional approaches focusing solely on physical aspects, PRT centers on the understanding that chronic pain often stems from neural pathways that have become maladapted, leading to the brain misinterpreting signals.
This innovative therapy doesn’t aim to ‘cure’ a physical problem, but rather to change the perception of pain. It teaches individuals to recognize that pain signals don’t necessarily equate to tissue damage. PRT achieves this through targeted interventions designed to reattribute pain to brain and mind processes, diminishing the perceived threat associated with bodily sensations.
The core principle involves accurately identifying and responding to what’s happening within the body, building a more adaptive and less fearful relationship with pain. It’s a relatively new approach, gaining traction due to its high success rates, particularly in conditions like chronic back pain, as demonstrated in recent clinical trials published in JAMA Psychiatry.
The Core Principles of PRT
Pain Reprocessing Therapy (PRT) rests upon several key principles. Firstly, it acknowledges that chronic pain isn’t always proportional to physical damage; the brain can generate pain signals independently. Secondly, PRT emphasizes the crucial role of the brain in perceiving and interpreting pain, rather than simply registering it.
A central tenet is the concept of neuroplasticity – the brain’s ability to reorganize itself by forming new neural connections. PRT leverages this to create new, healthier pain pathways. Furthermore, it directly addresses the fear-expectation-pain cycle, recognizing how anxiety and negative beliefs amplify pain sensations.
The therapy aims to reframe pain as a learned response, not an inherent defect, empowering patients to regain control. By challenging catastrophic thoughts and fostering emotional awareness, PRT helps individuals develop a more balanced and adaptive relationship with their pain experience, ultimately reducing suffering and improving function.
Understanding Nocebo and Placebo Effects in PRT
Pain Reprocessing Therapy (PRT) deeply considers the powerful influence of the nocebo and placebo effects on chronic pain. The nocebo effect demonstrates how negative expectations can increase pain, even without a corresponding physical cause. Conversely, the placebo effect highlights the ability of positive expectations to reduce pain.
PRT actively works to dismantle nocebo beliefs – often unconscious fears about movement or activity – that perpetuate the pain cycle. It doesn’t rely on trickery, but rather on educating patients about these phenomena and fostering a more optimistic outlook.
By reattributing pain to brain processes rather than structural damage, PRT aims to diminish the nocebo response. Simultaneously, it cultivates a sense of self-efficacy and hope, harnessing the body’s natural capacity for healing and amplifying the beneficial placebo response, leading to sustained pain relief.

The Theoretical Foundations of PRT
PRT’s core rests on neuroplasticity, recognizing the brain’s capacity to reorganize itself, and understanding pain as a complex brain-based experience, not solely tissue damage.
Neuroplasticity and Chronic Pain
Neuroplasticity, the brain’s remarkable ability to reorganize itself by forming new neural connections throughout life, is central to understanding PRT’s effectiveness. Chronic pain, often stemming from initially acute injuries, can become ingrained due to persistent neural pathways that amplify pain signals.

These pathways aren’t fixed; PRT leverages neuroplasticity to create new, adaptive pathways. By challenging pain-related beliefs and expectations, the therapy encourages the brain to reinterpret pain signals as less threatening. This process diminishes the amplification of pain and fosters a sense of control.
Essentially, PRT aims to “rewire” the brain, shifting from a state of chronic pain amplification to one of reduced sensitivity and improved function. This isn’t about denying the existence of pain, but rather changing how the brain processes and responds to it, ultimately breaking the cycle of chronic suffering.
The Role of the Brain in Pain Perception
Pain isn’t simply a sensory input traveling from the body to the brain; it’s a complex, constructed experience heavily influenced by brain activity. The brain actively interprets signals, factoring in past experiences, beliefs, and emotional states to determine the perception of pain.
PRT recognizes this crucial role, focusing on how the brain attributes meaning to pain signals. In chronic pain, the brain may mistakenly perceive harmless sensations as threatening, leading to persistent pain even after initial injuries have healed.
By re-attributing pain to non-threatening processes – like brain misinterpretations rather than tissue damage – PRT aims to recalibrate this perception. This shift in understanding reduces the brain’s alarm response, diminishing the intensity and suffering associated with chronic pain, fostering a sense of safety and control.
Breaking the Fear-Expectation-Pain Cycle
Chronic pain often becomes self-perpetuating, trapped within a vicious cycle of fear, expectation, and pain itself. Fear of movement or activity leads to heightened anticipation of pain, which, in turn, amplifies the actual pain experience. This cycle reinforces negative beliefs and behaviors, exacerbating the condition.
PRT directly targets this cycle by challenging maladaptive beliefs about pain. Through cognitive restructuring, patients learn to reframe their expectations, recognizing that pain doesn’t necessarily indicate harm.
Emotional awareness and processing are also key, as fear and anxiety significantly contribute to pain amplification. By addressing these emotional components, PRT helps patients break free from the cycle, fostering a sense of empowerment and enabling them to re-engage in life without constant fear of pain.
The PRT Treatment Process
PRT unfolds through a structured approach, beginning with comprehensive assessment and pain education, followed by cognitive techniques and emotional processing for lasting relief.
This therapeutic system retrains the brain, fostering accurate bodily awareness and diminishing the perceived threat associated with chronic pain sensations.
Initial Assessment and Pain Education
The PRT journey commences with a detailed initial assessment, meticulously evaluating the patient’s pain history, psychological factors, and beliefs surrounding their condition. This phase isn’t merely about identifying symptoms; it’s about understanding the unique narrative each individual constructs around their pain experience.
Crucially, pain education forms a cornerstone of this initial stage. Patients receive comprehensive information debunking the traditional “tissue damage = pain” model, particularly when dealing with nocebo and placebo effects. They learn about neuroplasticity, the brain’s remarkable ability to reorganize itself, and how this relates to chronic pain.
This education empowers patients to understand that their pain isn’t necessarily indicative of ongoing physical harm, but rather a result of altered brain processing. The goal is to reframe pain as a learned response, shifting the focus from a purely physical problem to one involving the brain and nervous system, paving the way for successful reprocessing.
Cognitive Restructuring Techniques
Cognitive restructuring lies at the heart of PRT, employing techniques to challenge and modify maladaptive thoughts and beliefs fueling the fear-expectation-pain cycle. Patients learn to identify negative thought patterns – catastrophizing, overgeneralization, and all-or-nothing thinking – that amplify pain perception.
Through guided questioning and exercises, these thoughts are examined for evidence, leading to the development of more balanced and realistic perspectives. This isn’t about positive thinking, but rather about accurate thinking, grounded in a nuanced understanding of pain mechanisms.
PRT utilizes techniques like thought records and behavioral experiments to test the validity of pain-related beliefs. By actively challenging these beliefs and experiencing the results, patients begin to unlearn ingrained patterns and cultivate a sense of control over their pain experience, ultimately diminishing its intensity and impact.
Emotional Awareness and Processing
PRT recognizes the profound link between emotions and pain, acknowledging that unresolved emotional distress can significantly contribute to chronic pain conditions. This component focuses on cultivating emotional awareness, helping patients identify and articulate feelings often intertwined with their pain experience – fear, anxiety, sadness, and anger.
Techniques like mindfulness and somatic experiencing are employed to facilitate a deeper connection with bodily sensations and associated emotions. Patients learn to observe these feelings without judgment, creating space for processing and release.
Exploring past experiences and traumas, when relevant, can uncover underlying emotional factors perpetuating the pain cycle. By addressing these emotional roots, PRT aims to reduce emotional reactivity and promote a more adaptive emotional response to pain, fostering overall well-being and pain reduction.

Evidence-Based Results & Clinical Trials
Rigorous clinical trials, notably in JAMA Psychiatry, demonstrate PRT’s efficacy, with two-thirds of patients experiencing significant or complete chronic back pain relief.
PRT consistently outperforms placebo and usual care, showcasing its potential as a transformative pain management approach.
Key Findings from the JAMA Psychiatry Study
The landmark study published in JAMA Psychiatry revealed strikingly positive outcomes for participants undergoing Pain Reprocessing Therapy (PRT). Researchers found that 66% (33 of 50) of individuals randomized to four weeks of PRT reported being either pain-free or experiencing near-complete pain relief post-treatment.
This contrasted sharply with the control groups, where only 20% (10 of 51) receiving placebo and 10% (5 of 50) receiving usual care achieved comparable results. The study highlighted PRT’s ability to facilitate a reattribution of pain, helping individuals perceive pain signals as less threatening, thereby diminishing the fear-expectation-pain cycle.
Professor Tor Wager, the senior author, emphasized the strong evidence supporting lasting pain relief through psychological intervention, specifically PRT. The research underscores the brain’s crucial role in chronic pain and the potential for retraining neural pathways to alleviate suffering.
High Success Rates in Chronic Back Pain
Chronic back pain sufferers experienced remarkable improvements through Pain Reprocessing Therapy (PRT), as demonstrated in recent clinical trials. A significant finding revealed that two-thirds of patients receiving PRT reported either the complete elimination or near-elimination of their chronic back pain – a result far exceeding expectations;
This substantial success rate positions PRT as a highly effective alternative to traditional pain management approaches. The therapy’s focus on retraining the brain to reinterpret pain signals proved pivotal in breaking the cycle of chronic discomfort.
Researchers, including Ashar and his team, observed that reattributing pain to mind or brain processes correlated directly with pain relief, offering a novel understanding of chronic pain recovery mechanisms and bolstering PRT’s efficacy.
PRT vs. Placebo and Usual Care
Comparative analysis reveals PRT’s superiority over both placebo and standard care in treating chronic pain. The randomized clinical trial showcased a striking difference: 66% of participants undergoing PRT achieved pain-free or near-pain-free status post-treatment.
This outcome dramatically contrasted with the 20% experiencing similar relief with placebo and a mere 10% benefiting from usual care. These findings strongly suggest that PRT’s effects extend beyond the placebo response, indicating a genuine neurobiological impact.
The study, published in JAMA Psychiatry, provides compelling evidence supporting PRT as a distinct and effective intervention. Professor Wager’s research underscores the potential of psychological treatment to deliver lasting relief, surpassing conventional methods.

Who Can Benefit from PRT?
PRT demonstrates efficacy for individuals with nocebo-driven conditions, particularly chronic pain where psychological factors significantly contribute to symptom presentation and persistence.
Suitable candidates often exhibit fear-avoidance behaviors and heightened pain expectations, benefiting from PRT’s targeted cognitive and emotional restructuring techniques.
Suitable Conditions for PRT
Pain Reprocessing Therapy (PRT) is particularly well-suited for conditions characterized by nocebo-driven pain, where negative expectations and fear amplify pain signals. This encompasses a range of chronic pain syndromes often considered “difficult to treat” with conventional methods.
Chronic back pain has shown exceptionally high success rates with PRT, as evidenced by recent clinical trials demonstrating significant pain reduction or elimination in a substantial portion of patients. Beyond back pain, PRT is being explored for conditions like fibromyalgia, tension headaches, and myofascial pain syndrome.
Conditions involving sensitized nervous systems, where the brain misinterprets signals as threatening, also respond favorably. PRT isn’t necessarily about “curing” a physical ailment, but rather retraining the brain to reinterpret pain signals, diminishing their emotional and behavioral impact. It’s crucial to note that PRT is most effective when pain isn’t primarily driven by structural damage or ongoing inflammation.
Identifying Candidates for PRT
Ideal candidates for Pain Reprocessing Therapy (PRT) often exhibit a history of failed conventional treatments and report significant distress related to their pain, despite limited objective evidence of structural damage. A key indicator is a strong belief that pain is driven by psychological factors or brain processes.
Individuals who demonstrate high levels of fear-avoidance behavior – limiting activities due to fear of pain – are also strong candidates. Those with a tendency towards catastrophizing or excessive worry about their pain may benefit significantly.
A thorough assessment by a qualified PRT practitioner is crucial. This includes evaluating pain history, psychological factors, and beliefs about pain. PRT is not a quick fix; candidates should be motivated and willing to actively participate in the therapeutic process, embracing cognitive and emotional restructuring techniques.
Contraindications and Considerations
While PRT demonstrates significant promise, it’s not universally suitable. Individuals with severe, untreated psychiatric conditions – such as active psychosis or severe depression – may require stabilization before commencing PRT. A comprehensive psychological evaluation is paramount.
PRT is not intended for acute injuries requiring immediate medical intervention. It’s best suited for chronic pain conditions where the pain persists beyond the expected healing time. Furthermore, individuals with unstable medical conditions should consult their physician.
Realistic expectations are crucial. PRT requires active participation and commitment; it’s not a passive treatment. It’s also important to acknowledge that pain reprocessing can initially lead to a temporary increase in pain as the brain recalibrates. Careful monitoring and support from a qualified practitioner are essential throughout the process.
Practical Aspects of Implementing PRT
Successfully implementing PRT necessitates locating a qualified practitioner, understanding the typical treatment duration (often several weeks), and considering accessibility and associated costs.
Treatment formats vary, encompassing individual sessions and potentially group settings, tailored to individual needs and preferences for optimal outcomes.
Finding a Qualified PRT Practitioner
Locating a skilled PRT practitioner requires diligent research, as this relatively new therapy isn’t yet widely available. Currently, a primary resource is the official Pain Reprocessing Therapy website, which maintains a directory of trained professionals.
Verify credentials by confirming the practitioner has completed comprehensive PRT training, ideally through programs directly affiliated with the developers of the therapy – Dr. Alan Gordon and Professor Tor Wager.
Consider experience; practitioners with a substantial history of successfully applying PRT to diverse patient populations are often preferred. Don’t hesitate to inquire about their specific experience with your condition.
Initial consultations are crucial for assessing compatibility and understanding the practitioner’s approach. A good fit involves feeling comfortable and confident in their expertise and communication style.
Beware of practitioners claiming PRT certification without verifiable training, as the field is still evolving and lacks standardized accreditation processes;
The Duration and Format of PRT
Pain Reprocessing Therapy (PRT) typically unfolds over a structured, time-limited course, commonly spanning 4-8 weeks. The initial phase involves intensive daily exercises, gradually transitioning to a maintenance schedule as progress is made.
The core format centers around daily online lessons and exercises, delivered through a dedicated platform. These modules focus on pain education, cognitive restructuring, and emotional awareness techniques;
Individual sessions with a qualified practitioner, usually conducted weekly, complement the online program. These sessions provide personalized guidance, address specific challenges, and reinforce learned skills.
Homework assignments are integral to PRT’s effectiveness, requiring consistent effort and self-application of the techniques outside of scheduled sessions. Active participation is key to achieving optimal outcomes.
The program’s flexibility allows for remote delivery, making it accessible to individuals regardless of geographical location, though in-person options may also be available.

Accessibility and Cost of Treatment
Accessibility to Pain Reprocessing Therapy (PRT) is expanding, largely due to the program’s adaptable format. The online delivery model significantly broadens reach, overcoming geographical barriers and offering convenience for patients.
However, finding a qualified practitioner remains a key factor. Resources like the Pain Reprocessing Therapy website and professional directories can aid in locating certified therapists.
The cost of PRT can vary, depending on the practitioner’s fees and the program’s structure. Typically, it ranges from $3,000 to $6,000 for a complete course of treatment.
Insurance coverage for PRT is currently limited, but advocacy efforts are underway to increase reimbursement rates. Some providers offer payment plans or sliding scale fees.
Self-guided resources, including workbooks and online materials, are emerging, offering a more affordable option, though professional guidance is generally recommended.

PRT and the Future of Pain Management
PRT represents a paradigm shift, moving beyond traditional approaches by addressing the brain’s role in chronic pain, offering hope for widespread adoption.
Ongoing research continues to refine PRT, exploring its mechanisms and expanding its application to diverse pain conditions, promising innovative advancements.
Compared to conventional treatments, PRT offers a non-invasive, psychological solution, potentially reducing reliance on medication and improving long-term outcomes.
Comparing PRT to Traditional Pain Treatments
Traditional pain management often relies on pharmacological interventions – pain medications – or physical therapies focused on addressing perceived structural issues. While these approaches can provide temporary relief, they frequently fail to address the underlying neurobiological mechanisms driving chronic pain, leading to limited long-term success and potential side effects.
Pain Reprocessing Therapy (PRT) distinctly differs by targeting the brain’s interpretation of pain signals. Instead of focusing on the physical source, PRT aims to retrain the brain to perceive these signals as less threatening. This psychological approach bypasses the limitations of solely addressing physical symptoms.
Unlike treatments that may inadvertently reinforce fear-avoidance behaviors, PRT actively challenges these beliefs, fostering a more adaptive and positive relationship with bodily sensations. This can lead to more sustainable pain reduction and improved functionality, offering a potentially transformative alternative for many individuals struggling with chronic pain conditions.
PRT’s emphasis on neuroplasticity and cognitive restructuring sets it apart, providing a holistic and empowering approach to pain management.
The Potential for Widespread Adoption

Widespread adoption of Pain Reprocessing Therapy (PRT) hinges on increasing awareness among healthcare professionals and the public. The compelling results from recent clinical trials, particularly the JAMA Psychiatry study demonstrating high success rates in chronic back pain, provide a strong foundation for integration into mainstream pain management.
However, several factors need addressing. Training a sufficient number of qualified PRT practitioners is crucial, alongside developing accessible and affordable treatment options. Overcoming existing biases towards psychological approaches for chronic pain is also essential.
Further research into the mechanisms of PRT and its efficacy across diverse pain conditions will bolster confidence and encourage broader implementation. Telehealth delivery models could significantly enhance accessibility, particularly for individuals in remote areas or with limited mobility. Ultimately, PRT’s potential lies in offering a paradigm shift – a move towards brain-focused, empowering pain care.

Ongoing Research and Development in PRT
Current research endeavors are focused on elucidating the precise neural mechanisms underpinning PRT’s effectiveness. Investigations are exploring how cognitive restructuring and emotional processing impact brain activity and pain perception, utilizing neuroimaging techniques to map these changes. A key area of study involves identifying biomarkers that predict treatment response, allowing for personalized PRT protocols.
Researchers are also expanding the application of PRT to a wider range of chronic pain conditions beyond back pain, including fibromyalgia, migraines, and neuropathic pain. Development of standardized PRT protocols and therapist training programs is underway to ensure treatment fidelity and quality control.
Future directions include investigating the integration of PRT with other therapies, such as physical therapy and mindfulness-based interventions, to optimize outcomes. The goal is to refine PRT into a robust, evidence-based treatment option readily available to those suffering from chronic pain.